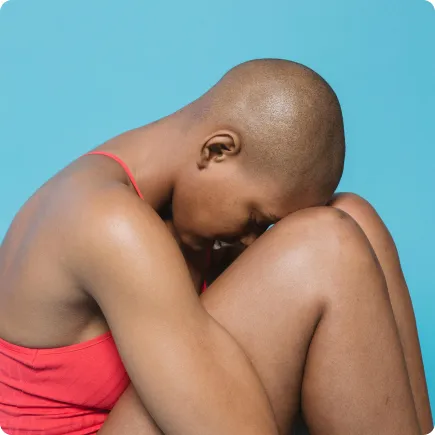
Menopause and Depression

What is depression in menopause?
Depression is a common and serious medical illness that negatively affects how you feel, think, and act.
If you are in crisis, please call 988 for the Suicide and Crisis Lifeline or text HOME to 741741 to reach the Crisis Text Line. You are not alone, and there is help available.
What causes depression during?
Research suggests that a person’s genetics, personality, life stressors, medical history, medications, and brain biochemistry cause depression.
One reason depression may occur at higher rates during perimenopause and menopause is because of the decreasing levels of estrogen and progesterone—which lead to changes in mood.
Some researchers think that there is a “window of vulnerability” during perimenopause when some women are susceptible to the effects of fluctuating hormones, especially if they have experienced depression before.
Additionally, other symptoms associated with perimenopause and menopause can create conditions conducive to depression—like hot flashes causing sleeplessness, which increases the likelihood of depression.
of Members report symptom improvement within 3 months.
care at your fingertips.

What is happening inside your body?
Depression is linked to shifts in activity in different parts of your brain, like the hippocampus, amygdala, thalamus, and prefrontal cortex, which regulate mood and cognition. Fewer connections between neurons are also observed in these areas in people with depression.
Neurotransmitters have a significant role in depression as well. When there is a disruption in communication between neurons, there can be issues with levels of serotonin, epinephrine, glutamate, GABA, acetylcholine, and norepinephrine.
How is depression diagnosed during menopause?
Once paired with your provider, they will diagnose you based on the description of your symptoms.
What are some medical-provider-prescribed treatments for menopause-related depression?
Antidepressants: Selective serotonin reuptake inhibitors (SSRIs) are the most commonly used antidepressants; they increase the amount of serotonin in the brain, improve mood, and reduce anxiety.
Hormone replacement therapy: By restoring estrogen levels, this type of therapy can help treat emotional changes, including mild or moderate depression.
of Members report symptom improvement within 3 months.
care at your fingertips.

What are some non-medical treatments for coping with depression in menopause?
- Psychotherapy: This type of talk therapy can be one-on-one or in a group setting and often goes hand in hand with medication. Forms of psychotherapy include cognitive behavioral therapy and interpersonal therapy. We recommend Thrive Psychology, Grow Therapy, and Happier Living as mental health partners.
- Mindfulness: This involves focusing the mind on the present moment rather than on the past or future. Some research has shown it helps alleviate depression and also rewires the brain.
- Exercise: Physical activity helps improve mood through the release of endorphins which trigger positive feelings—it can also boost self-esteem.
- If you are in crisis, please call 988 for the Suicide and Crisis Lifeline or text HOME to 741741 to reach the Crisis Text Line. You are not alone, and there is help available.
Can depression during menopause be prevented?
- If yes, how
- Emphasis on the importance of seeking treatment
What should you do next?
Let’s get you prepared to be paired with your provider!
Select and submit all of the symptoms you are currently experiencing so your doctor can assess and provide a tailored treatment plan for you.
For additional support, reach out to the Crisis Text Line or Suicide Crisis Lifeline.
of Members report symptom improvement within 3 months.
care at your fingertips.

References
- A 2018 review published in the journal Obstetrics and Gynecology Clinics of North America showed that women are up to five times more likely to experience a depressive disorder during perimenopause than during the period immediately before perimenopause.
- Up to 40% of women going through perimenopause experience depression, suggested a study on Turkish women published in the journal Menopause in 2010.
- Despite reported high rates of depression, a 2020 study also published in Menopause found that 34.1% of OB-GYNs don’t typically screen perimenopausal patients for this illness.




