Is Spotting Normal After Menopause?

After menopause, you may notice unexpected vaginal bleeding (i.e. spotting). This type of bleeding is referred to as postmenopausal bleeding. And while the causes may not be serious and are typically benign, it’s never something you should ignore. In this piece, we’ll explore why spotting may occur after the menopause transition—and why you should always discuss it with your healthcare provider.
Spotting After Menopause: Possible Causes
The average age of menopause is 51, but it can occur years earlier or later. After menopause, you no longer ovulate which means that your periods stop. So what could cause spotting? As we’ll see shortly, there are a range of illnesses and mild injuries that could be responsible.
Roughly 10% of postmenopausal women experience spontaneous vaginal bleeding in the first couple of years following their final menstrual period. And while you may feel concerned if you find yourself in that 10%, bear in mind that the most serious underlying issues are also less common (although, this does not give you a pass to ignore postmenopausal bleeding!). Let’s review some of the possible causes of spotting during menopause.
You’re Not Actually in Menopause Yet
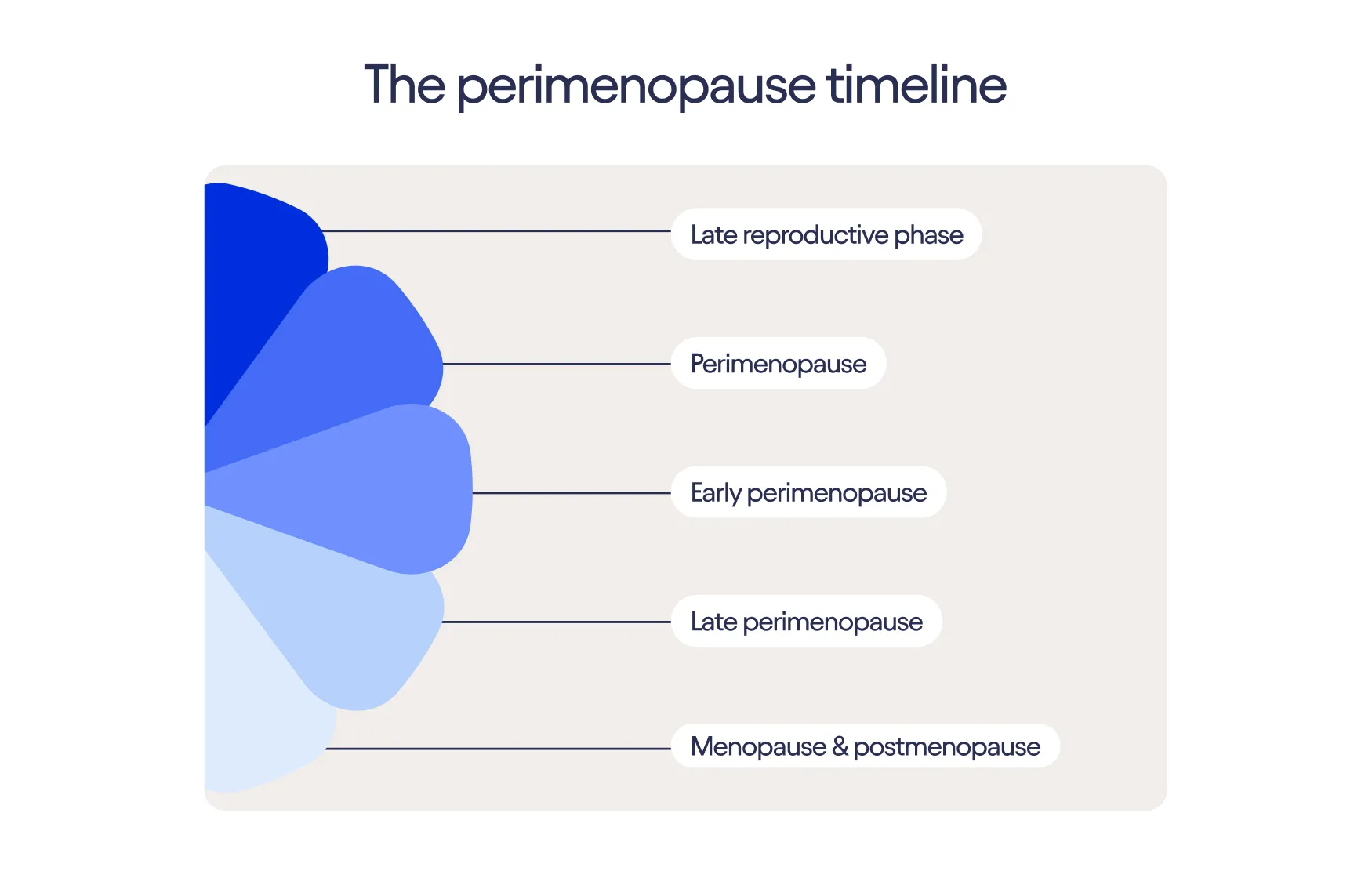
You have officially reached menopause 12 months after your final menstrual period. Leading up to this, your periods may become progressively more irregular and sporadic. It’s not uncommon during this time to skip one or several periods and then resume menstruating. So if you seem to be spotting after what you believe is your final menstrual period, there’s a possibility that you are actually still in perimenopause.
Genitourinary Syndrome of Menopause (GSM)
Throughout the menopause transition, your production of estrogen drops, which has a major effect on your entire body. Your vagina, vulva, and urinary tract—which are especially rich in estrogen receptors—are particularly impacted, as falling estrogen causes the tissues to grow thinner and more fragile.
This is called the genitourinary syndrome of menopause (GSM), and it makes up a constellation of some of the most common menopause symptoms. GSM causes vaginal dryness and irritation. It also increases the risk of minor injuries (such as small cuts and tears) from penetrative sex, which can lead to bleeding or spotting.
Urinary Tract Infection (UTI)
Urinary tract infections (UTIs) become more common both during and after the menopause transition due to falling estrogen levels and changes affecting the tissues of the urinary tract. UTIs can sometimes lead to blood in your urine, which you might mistake for vaginal bleeding.
Hemorrhoids
Hemorrhoids—i.e. swollen veins in your anus and rectum—are more likely to appear during menopause for several reasons. First, aging is a hemorrhoid risk factor for everyone. The tissues of your anus tend to weaken and stretch over time, allowing the veins to become distended. Second, shifting hormones may change your digestion patterns during menopause, causing constipation. And if you’re constipated, straining to have a bowel movement can trigger hemorrhoids.
Hemorrhoids can cause light bleeding when you have a bowel movement. This can show up as blood on your toilet paper, which you might mistake for vaginal spotting.
Endometrial Polyps
Endometrial polyps are small, soft growths that may appear on the inner lining of your uterus (the endometrium). These growths can irritate the surrounding tissue, leading to vaginal bleeding and spotting. They affect about 8% of women in the general population. After menopause, however, they become significantly more common, affecting about 20% of women. Roughly two thirds of those who do have endometrial polyps will experience abnormal bleeding, regardless of age. Although 1% of endometrial polyps can be cancerous, the vast majority are benign (non-cancerous) and result from an overgrowth of cells in the endometrial lining.
Endometrial Hyperplasia
Endometrial hyperplasia develops when an imbalance of estrogen and progesterone causes the lining of the uterus (endometrium) to thicken. This overgrowth of tissue often leads to postmenopausal bleeding. Some forms of endometrial hyperplasia can evolve into cancer, so it’s very important to address any postmenopausal bleeding immediately.
Cervicitis
The cervix is a muscular, neck-like organ that separates the uterus from the vagina. An inflammation of the cervix—called cervicitis—can cause vaginal bleeding and spotting. It may also be associated with frequent urination, pain during sex, and bleeding after sex. Cervicitis can affect anyone who has a cervix, regardless of age or reproductive status.
Cervicitis may be triggered by many different underlying issues that can arise both before and after menopause. That includes bacterial infections (like bacterial vaginosis), sexually transmitted infections (such as chlamydia and gonorrhea), and chemical irritation (e.g. from spermicide or vaginal douches).
Sexually Transmitted Infection (STI)
Sexually transmitted infections (STIs) like chlamydia and gonorrhea are a well-established cause of unexpected vaginal bleeding. They can also cause vaginal pain, itching, discharge, and pain during urination. STIs are caused by bacteria or viruses that spread through genital, oral, or anal contact between you and your sex partner(s).
Anyone who is sexually active can contract a sexually transmitted infection (STI) including people in menopause. That means you still need to protect yourself against STIs, even if you can no longer get pregnant and don’t need to use contraception. It’s also important to get tested regularly and discuss safer sex practices with your sex partners. Using barrier protection when you have sex, such as male or female latex condoms, is an effective way to prevent the transmission of STIs.
Cancer
Another potential cause of spotting after menopause is uterine (endometrial) or ovarian cancer. The good news is that most postmenopausal bleeding is not caused by cancer. One study showed it was responsible for just 6.6% of these events.
Even so, the prospect of such a serious illness should always be taken seriously. Endometrial cancer is more common after menopause, and frequently causes bleeding. That’s why you should speak with your doctor about any unexplained vaginal bleeding. Remember—the sooner you receive treatment, the better your outcomes are likely to be.
Menopausal Hormone Therapy (MHT)
Menopausal hormone therapy (MHT) is a safe and effective treatment for many menopause symptoms. MHT uses a synthetic form of estrogen to supplement your natural hormone levels. This estrogen helps restore normal function to your tissues and organs, including your brain, skin, bones, and genitals. As discussed above, doctors will often prescribe progesterone along with the estrogen. This helps prevent a thickening of the endometrium. But it can also occasionally cause the endometrium to grow too thin, which leads to light vaginal bleeding.
If you’re taking MHT and noticing spotting, let your healthcare provider know. After ruling out more serious causes, they can lower your progesterone dose to prevent bleeding in the future. It may take a few tries to find the right dose for you, so try not to get discouraged!
How Is Spotting After Menopause Diagnosed?
If you’re noticing spotting after menopause, it’s important to let your healthcare team know right away. In most cases, your healthcare provider will have you come in for an examination. Depending on how you describe your symptoms, they may run a number of tests, including:
- Pelvic exam: The doctor examines your vulva, vagina, cervix, uterus, and ovaries for anything unusual. They will both look and feel for abnormalities and will probably use a tool called a speculum to see inside your vagina.
- Pap smear: The doctor collects cells from your cervix by gently scraping it. These cells are then examined for signs of illness.
- Pelvic Ultrasound: This screening test (done with an abdominal and/or vaginal probe) uses sound waves to create an image of your internal organs. It can help diagnose abnormalities of your uterus and ovaries (such as ovarian cysts or masses, endometrial polyps, or endometrial thickening.
- Endometrial Biopsy: Done in the office setting, the healthcare provider inserts a thin catheter through the cervix into the endometrial cavity in order to collect a small sample of tissue for further testing.
- Hysteroscopy: Done in either the office setting or the operating room, your healthcare provider inserts a device (hysteroscope) through your cervix and into your uterine cavity and then distends the cavity with fluid. The hysteroscope has a light at the end that helps your healthcare provider look for abnormalities. It also allows them to take biopsies or remove any concerning lesions.
- STI tests: Your healthcare provider uses a sample of blood, urine, or a genital swab to look for STIs, like chlamydia and gonorrhea.
Depending on what these tests reveal, your healthcare provider can give you a diagnosis and determine what, if any, additional interventions (e.g., surgery) are needed.
The Bottom Line
Postmenopausal bleeding can happen and, although the causes are typically benign, it’s not something you should ever ignore. If you’re experiencing any unexplained bleeding after menopause, please talk with your healthcare team right away and get to the bottom of it.